Even though symptoms for gestational diabetes are nothing to be alarmed about unless they continue past the pregnancy, women should still carefully monitor their blood sugar levels. Maintaining normal glucose levels during pregnancy helps reduce health risks and ensures a healthy condition for both mother and baby.
Gestational diabetes often appears silently, which makes routine testing critical for early diagnosis and treatment. A glucose challenge test or glucose tolerance test is typically conducted between weeks 24 and 28 of pregnancy to screen for high blood sugar levels. Early detection during these weeks allows healthcare providers to implement dietary changes or insulin treatments that minimize risks. Pregnant women with higher risk factors may be tested even earlier in their pregnancy to manage their blood glucose levels effectively.
Prenatal care begins with appointments to the healthcare provider as soon as the woman realizes she is pregnant. Prenatal care is important for both the health of the pregnant woman and the health of the soon-to-be-born baby. Gestational diabetes testing is a standard part of routine prenatal care, helping providers assess blood sugar levels even in cases where the woman is not experiencing typical gestational diabetes symptoms.
What Gestational Diabetes is And Why It’s Important
Gestational diabetes is a condition that occurs in women during pregnancy, characterized by high blood sugar levels. It can manifest symptoms similar to both type 1 diabetes and type 2 diabetes. Gestational diabetes does not occur in all pregnancies, only in less than 5% of cases. However, studies have shown that gestational diabetes rates in the U.S. have risen over the years, and now approximately 8%-10% of pregnant women develop this blood sugar condition. Worldwide, the rate can be even higher due to factors such as lifestyle, age, ethnicity, and access to healthcare. These trends highlight the importance of early screening and provider intervention to manage and prevent health risks.
The condition usually disappears or shows signs of improvement after the woman has given birth, although in almost half of the cases, the woman ultimately develops type 2 diabetes later on. Managing blood sugar levels during and after pregnancy is crucial for long-term health. Gestational diabetes can occur in women who have not experienced any form of diabetes in their lives before, increasing their risk of developing diabetes-related health problems in the future.
Gestational diabetes may be temporary, but it can significantly affect the health of both the mother and the baby if left unmanaged. High blood sugar levels during pregnancy increase the risk of the fetus developing anomalies in the central nervous system and cardiac system. Additionally, babies may be born with higher or lower birth weights and may have malformations in the skeletal and muscular systems. Other complications include respiratory distress syndrome, inhibited production of fetal surfactant, and destruction of red blood cells, posing serious health problems for the newborn.
Symptoms of Gestational Diabetes
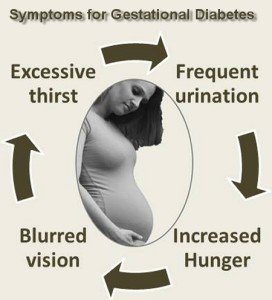
Gestational diabetes may sometimes present symptoms like a feeling of excessive thirst, leading to increased fluid intake. High blood sugar levels (glucose) cause frequent urination, similar to symptoms seen in type 1 and type 2 diabetes. However, in most cases, gestational diabetes does not cause easily noticeable symptoms, making it a significant health risk as it can go undiagnosed. Some pregnant women may experience mild symptoms such as tiredness and nausea alongside excessive thirst and frequent urination, but these can often mimic normal pregnancy-related changes. This is why regular screening tests during prenatal care are vital to manage blood sugar levels and ensure a healthy pregnancy outcome.
Medical practitioners, including healthcare providers, need to constantly monitor pregnant women, especially after their 5th or 6th month, for any signs of gestational diabetes. Regular blood sugar tests and glucose level assessments are essential to ensure timely detection and management of the condition.
Treating Gestational Diabetes
Actually, gestational diabetes will normally disappear or lessen several weeks after the woman has given birth. The pregnancy-related hormones that were affecting her blood glucose levels will have been cleared by then. However, there is a significant risk of the woman developing type 2 diabetes later in life after having gestational diabetes. This risk is influenced by her genes and lifestyle. Maintaining a healthy lifestyle, including proper diet and exercise, can help manage blood sugar levels and prevent the development of diabetes. Smoking is a risk factor for diabetes and can cause complications, posing dangers to both the mother’s body and the fetus, and should therefore be avoided.
In cases where dietary management is insufficient to control blood sugar levels, healthcare providers may prescribe insulin or other medications as part of the treatment plan. Patients are typically required to record their blood sugar levels at regular intervals—such as before meals and one to two hours after eating—to track glucose trends and manage their condition effectively. Small changes to the diet, such as adding whole grains, switching to low-fat dairy, and avoiding sugary snacks, along with regular exercise, can play a significant role in maintaining normal glucose levels and promoting overall health.
Many medical practitioners recommend controlling weight gain and carbohydrate intake during pregnancy to help defray gestational diabetes. Managing blood sugar levels during pregnancy is essential for maintaining both the mother’s and baby’s health. Expectant mothers should be extra careful regarding their condition, especially if they come from a family with a higher risk of diabetes. Genetics play a vital role in diabetes of any type or kind. If you suspect that you may be susceptible to gestational diabetes, do not hesitate to consult your obstetrician during your next appointment regarding necessary tests and management strategies.
Gestational Diabetes Risks
There are certain risk factors that can increase a woman’s likelihood of developing gestational diabetes. If you meet any of the following conditions, you have greater odds of developing this diabetes-related condition:
- You’re over 33 years of age, increasing your risk of gestational diabetes.
- You’re overweight or obese. Higher weight increases your odds of developing diabetes during pregnancy.
- You’ve had gestational diabetes before
- You’re of African American, Indian, Hispanic, or Asian descent, which are higher risk groups for diabetes.
- You are a smoker, which increases the risk of diabetes complications.
Additional risk factors for gestational diabetes include a history of polycystic ovary syndrome (PCOS), prediabetes, or having delivered a baby weighing more than 9 pounds in a previous pregnancy. Overweight women above age 25 and those of specific ethnic backgrounds, including Native American and Pacific Island descent, are also at higher risk of developing diabetes during pregnancy.
If you are concerned, once you’re pregnant, schedule an appointment with your healthcare provider to have a gestational diabetes test done. Early testing helps manage blood sugar levels and maintain a healthy pregnancy.
Gestational Diabetes Meal Plan
If you are diagnosed with gestational diabetes, your doctor or healthcare provider will likely recommend a special diabetes meal plan. Each doctor or dietician may have their own dietary preferences, but the diet will focus on limiting the amount of carbohydrates that you eat. Proper eating habits, including managing carbohydrate intake, help keep blood sugar levels normal. We all need some carbohydrates, but consuming too much in too short a time can raise your blood sugar to unsafe levels. Most pregnant women will be able to control their gestational diabetes with their diet, but your doctor may determine that you need additional help in the form of insulin or other medications. It’s important not to self-medicate; let your healthcare provider guide your treatment plan to manage blood sugar levels effectively.